Physics of Thermal Therapy
Free download. Book file PDF easily for everyone and every device. You can download and read online Physics of Thermal Therapy file PDF Book only if you are registered here. And also you can download or read online all Book PDF file that related with Physics of Thermal Therapy book. Happy reading Physics of Thermal Therapy Bookeveryone. Download file Free Book PDF Physics of Thermal Therapy at Complete PDF Library. This Book have some digital formats such us :paperbook, ebook, kindle, epub, fb2 and another formats. Here is The CompletePDF Book Library. It's free to register here to get Book file PDF Physics of Thermal Therapy Pocket Guide.
Contents:
As expected, the maximum temperature rise is observed on the line of focal symmetry,. A step increase from zero to either 3.
The phantom was allowed to reach thermal equilibrium before changing the power input. MRI thermal images collected for the case of 6. The validation datasets, consisting of the images collected during the experiments with the other two power levels, were used to assess the adequacy of the identified basis functions and the accuracy of the temperature predictions obtained with the identified ultrasound treatment model. A total of MR thermal images were acquired to characterize temperature evolution during each power step test.
The estimation dataset included images collected when the power was kept constant at 6. Figure 4 a shows the measured temperature elevation within the ROI at s when the temperature reaches its peak value. The temporal evolution of temperatures in the selected locations on the line of ultrasound beam symmetry is shown in Figure 4 b. The highest temperature was observed at , where the maximum temperature increase from ambient temperature was C.
All images in the estimation dataset were used to identify the orthonormal basis following the described method. Figure 5 shows the first four identified eigenfunctions and the corresponding eigenvalues, which rapidly decay for the higher order 's. Using the criterion 9 , it was determined that the first eigenfunction captures approximately of the spatial correlations in the collection of images, while captures only. Selecting , we conclude that high accuracy of image approximations in the reduced POD basis is achieved with only two basis functions.
Society for Thermal Medicine > HOME
Note that the shape of , identified to maximize the explained spatial correlations in thermal images, is similar to the shape of temperature distribution, as expected. Further note that eigenfunctions , capture information at increasingly higher spatial frequencies, and that ignoring their contribution in image representation 15 has the effect of a spatial filtering of imaging data. Thermal images, collected during tissue cooling after the initial sonication at 6. The result of Table 1 was obtained by, first, using Matlab's System Identification Toolbox [13] to obtain the autoregressive model of the cooling process and then converting it into the state space form of equation Sequential thermal images were used in equation 22 to estimate the power deposition projection.
The identified vector Table 1 was then used in equations 13 to estimate ; the corresponding was obtained using equation The result SAR , scaled with the total applied power of 6. A high degree of correlation between the shapes of the measured temperature distribution Figure 4a and the SAR is an expected result for the unperfused phantom. The result is shown after pointwise scaling of SAR with 6.
The prediction of the thermal response to different power inputs is based on the assumption that the shape of the SAR remains constant for the fixed relative transducer-patient position, but the SAR values are scaled with the applied electrical power.
- Fundamentals and Clinical Applications, 1st Edition?
- Thermal therapy techniques for skin and superficial tissue disease;
- The Desire and Pursuit of the Whole.
- Cartooning: Character Design.
Figures 6 b and c shows the difference between the predicted and the directly identified SAR , both scaled to 1W of the applied power. Low prediction errors confirm that in our experiments the specific absorption rate changed linearly with the applied power.
Submission history
The accuracy of the identified reduced-order treatment model was assessed in projection manifold and in terms of temperature predication errors. In projection space, the prediction of the temperature projection vector , obtained with the same two-dimensional state space model of Table 1 and the appropriately scaled , was compared with the projection of the actual thermal images , acquired during the experiments with three different power levels. Image projections, , were found as the least squares solution of equation Figure 7 shows an excellent agreement between the predictions, , and measurements,.
The agreement is the best for 6. The plot of is similar in shape to the pointwise temperature evolutions cf. Figure 4b , which indicates that the first component of the vector captures most of the slow temporal variations in the series of thermal images. The projections, , of the acquired images are compared with model predictions, , obtained with the identified thermal response model.
The value of listed in Table 1 was used to make predictions for the case of 6. Predictions for the power inputs of 3. When used in equation 15 , the model-generated gives the prediction of the temperature elevation, , in the ROI, which can be compared with imaging data,. Figure 8 shows the spatial mean and standard deviation STD of the temperature prediction errors for all pixels in the ROI. The prediction errors are small, including the two validation cases shown in subplots a — d.
The maximum pointwise temperature prediction errors do not exceed C, which is of the same order as the measurement noise of MRI thermometry. Graphs a — b show the results for 3.
The developed approach was shown to be effective in identifying low-dimension but accurate models of ultrasound thermal therapies. At a pre-treatment stage, a set of MR thermometry images, characterizing the response of the target and the surrounding normal tissue to thermal excitation, is collected and then used to identify the reduced POD basis, which capture spatial correlations in images. A simple criterion for selecting an appropriate number of basis functions is provided which allows a user to balance the computational complexity of a predictive treatment model with its computational complexity.
The selected reduced basis is then used to parsimoniously approximate newly acquired images, thus minimizing storage and data traffic.
Search form
As an additional benefit, image approximation in the reduced basis filters high-frequency spatial noises in MR images. The SAR and thermal response models identified following the developed approach are patient- and site-specific and can be used as predictive models in real time e. The identification procedures are well suited to perform continuous re-identification of treatment models during the therapy. Such intra-treatment adaptability helps to mitigate the effect of changing tissue properties such an US absorption and blood perfusion, caused by elevated temperatures, on the accuracy of model predictions, which is particularly important when the identified low-dimensional models are used to efficiently implement model-based, optimizing treatment controllers that utilize images in the feedback.
A family of related results used to identify continuous-time treatment models is described in reference [19]. The developed methods were validated during in vitro MR experiments with a tissue phantom heated by a focused ultrasound transducer. The experimental results indicate that the SAR and thermal response during the treatment can be accurately predicted by the identified projection models with only two states.
The low-dimensionality of the identified models substantially minimizes computational requirements of implementing a model-based treatment control system and communication traffic between the MRI scanner and the treatment controller.
Thermal Oncology Program
Though our emphasis is on thermal therapies, the developed approach has a broader applicability in image-based identification and image-guided control of therapies. After straightforward modifications, this approach can be used with images acquired in multiple planes and with three-dimensional MR measurements. Conceived and designed the experiments: MS. Performed the experiments: RN MS. Analyzed the data: RN MS. Wrote the paper: MS. Browse Subject Areas? Click through the PLOS taxonomy to find articles in your field.
- Physics of Thermal Therapy: Fundamentals and Clinical Applications - Google книги;
- Physics of Thermal Therapy: Fundamentals and Clinical Applications.
- Chris Diederich.
- The Cavendish Laboratory 1874–1974.
- Knowledge, Power and Educational Reform: Applying the Sociology of Basil Bernstein.
- The Good Husband of Zebra Drive (No. 1 Ladies Detective Agency, Book 8).
- See a Problem??
Abstract Medical imaging provides information valuable in diagnosis, planning, and control of therapies. Introduction In ultrasound US thermal therapies, the goal is to selectively heat the treatment target without excessively elevating the temperature in healthy tissues intervening in the path of transmitted US energy and surrounding the target. The selected reduced basis is then used to: Approximate each image acquired during therapy in the reduced set of basis functions. This step may be viewed as a real time image compression, which exploits spatial correlations of image voxels, as well as the image filtering step since high-frequency spatial valuations, which usually correspond to MRI measurement noise, are removed.
Identify the ultrasound specific absorption rate and the dynamic model that captures temporal correlation in the series of images and provides a prediction the evolution of the ultrasound treatment. Methods Identification of basis functions using POD method The proper orthogonal decomposition is a technique often used to extract a set of basis functions for an approximate, modal-like representation of an infinite-dimensional, distributed parameter system DPS.
Image representation in the reduced basis Consider a thermal image , collected at time , which reflects the spatial temperature distribution in the region of interest in response to the sonication history over the time.
Representation of ultrasound power deposition The temperature distribution measured by MR thermometry depend on the power deposition in tissue, in W m , caused by sonication. Identification of the projection models of thermal response Our objective is to to identify an ultrasound thermal treatment model in a low-dimensional projection form with the state vector, , corresponding to the projection of measurements,.
At Last a More Effective, More Humane Solution for Treating Cancer.
Download: PPT. Figure 1. Treatment control system uses low-dimensional projection models of the therapy and the SAR. Identification of matrix. Identification of the affine term. Results The developed approach to identifying low-dimensional models of ultrasound therapies was tested experimentally using MR measurements of the thermal response of a tissue phantom to focused ultrasound FUS sonication.
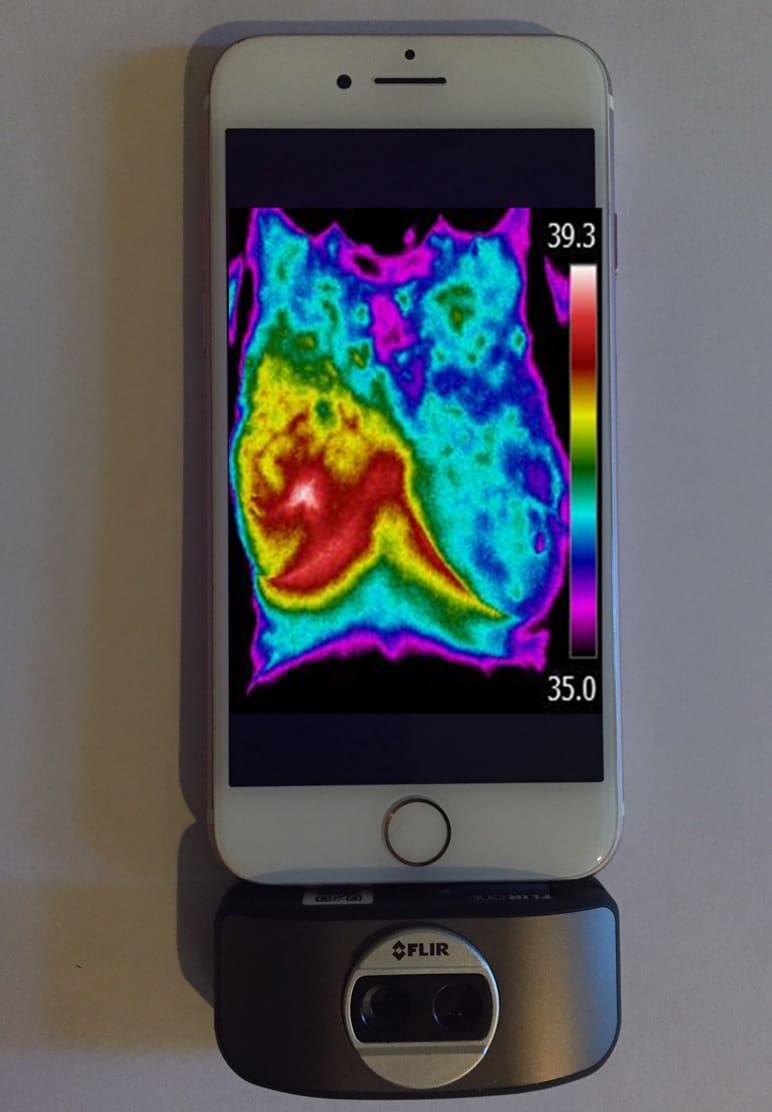
Figure 2. MR-compatible ultrasound transducer and positioning system. Figure 3. Coronal MRI map of temperature elevations inside the phantom heated by focused ultrasound transducer. Validation Results A step increase from zero to either 3.
- PQ : how it matters more than IQ
- The Warning (Sarah Roberts, Book 2)
- Man Up!: 367 Classic Skills for the Modern Guy
- My Guantanamo Diary: The Detainees and the Stories They Told Me
- Gender, Culture and Organizational Change: Putting Theory into Practice
- Cubed Foot Gardening: Growing Vegetables in Raised, Intensive Beds